Challenges to Better Healthcare access in Bangladesh Urban Slums
Introduction
Bangladesh is known to be the seventh most densely populated country in the world having a population of more than 150 million people inhabiting an area of 147,570 square kilometers (BBS 2011; UNFPA 2011). It hosts one of the fastest growing megacities around the world of populations over 10 million people with enormous and expeditious urbanization occurring during the past 40 years. The population has also grown exponentially from 5% to 28% reckoning to 45 million people and about 50% of Bangladesh’s population is expected to live in Urban areas by 2050 (United Nations, 2012). These are speculated to be mainly migrants in lieu of better services, employment, and disaster relief (The Geographical Review, 1982). However, the opportunities in the urban spaces keep growing geometrically despite the exponential growth of the population as shown in Fig.1. As a result, many are being left out without an opportunity, giving rise to ambiguous poor urban populations and slums (The Lancet, 2013). The fast and rapid urban population densification is welding unmanageable pressure on urban infrastructure and resources pessimistically building on habitability (Ahmed, 2014). Health is one of the most constrained resources in urban areas and within the urban slums, many lack access to better healthcare services. Despite the several successes recorded in the healthcare sector, The Lancet (2013) states that the daunting challenge is to provide better healthcare for poor people in urban areas, as they make up the majority of slum dwellers who account for about 14,000 slum settlements that were counted by the government in 2014 (World Bank, 2018). According to the Universal Declaration of Human Rights in 1948, better healthcare is every person’s right and it implies access to adequate food, clothing, housing, medical care, and social services. It also states that everyone has a right to protection from unemployment, illness, disability, widowhood, old age, or other deficiency of livelihood which is beyond his or her control (Human Rights Declaration, 1948, Article 25/1). It is important to note that the Local Government Division is responsible for the provision of primary healthcare services to poor urban populations and it is unable to meet the demands adequately. This paper examines the challenges to better healthcare access in urban slums with a deeper analysis of the health systems, current situations in slums, and initiatives in place.
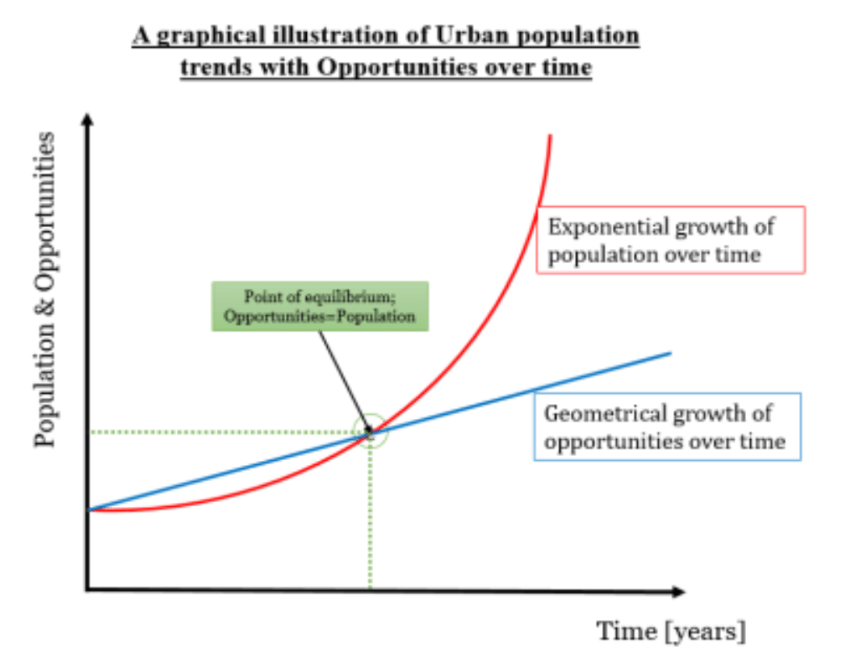
Fig. 1. Created by Author
Methodology
This paper is dependent on a narrative approach, as it uses mixed methods of data collection that are both primary and secondary. The primary data was collected through a structured questionnaire survey using Google Docs and 56 responses were evaluated with a majority of 51.8% having been through urban slum areas and 5.4% residing in slums. The secondary data has been collected from secondary sources based on analysis of various types of documents regarding urban slums, health accessibility, and current needs. This includes sources such as articles, newspapers, books, journals, reports, and websites regarding health accessibility.
Analysis
Graphical Data Analysis
The data collected from the survey in Fig. 2 proved the hypothesis that access to better healthcare services in Bangladesh’s Urban Slums is a challenge. The graphical illustration below shows that the major stakeholders in ensuring better healthcare access to the urban poor in Bangladesh’s urban slums are the government ministries, the Non-government organizations, the populations in Urban slums, and healthcare workers, who have not yet performed to the utmost expectation. Government Ministries are expected to play a vital role in ensuring better healthcare access but have been highly skewed towards the left, which accounts for insufficient efforts at that modal, implying that the government is off the radar if the graphical data is to be represented in normally distributed curves. The non-government Organizations (NGOs) have a normally distributed effort but since they are inadequate, they have played a big role in ensuring better healthcare accessibility in Bangladesh’s urban slums through operations such as the BRAC MANOSHI. The efforts played by the populations in urban slums show some disjointness but this may be because of variability among the populations, nevertheless, the graphical illustration takes a moderate negative skewness with the mode standing at a weak point, meaning that their efforts were close to satisfactory but not entirely; there is a lag somewhere. The health workers have an approximately normal effort distribution with a low variability given a moderate mode that stands at average, however, some claim that there is a proportion pending within the health workers.
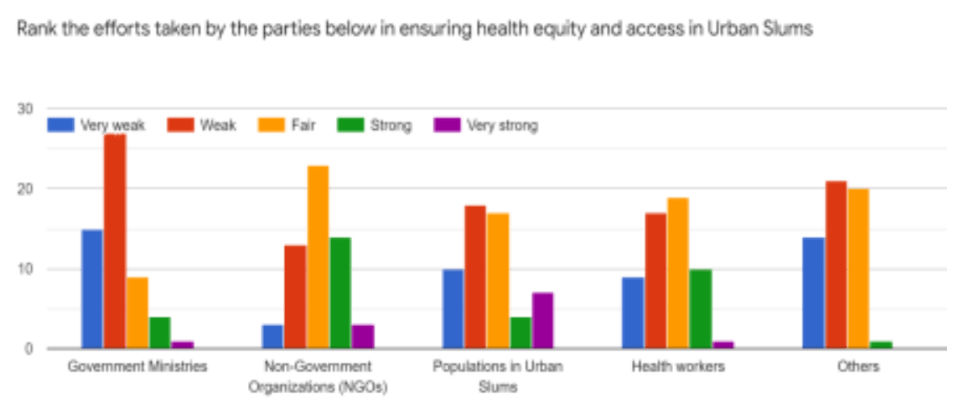
Fig. 2. Created by Author
Other factors have also played a big role in making it hard to access better healthcare services and this paper shall get into some of such strands. Secondary sources show that poverty, ignorance about better healthcare services, and unavailability of health resources are some of the key facets hindering better healthcare accessibility in the urban slums of Bangladesh.
Other limiting factors in details
Poverty has been listed as one of the major limiting points to better healthcare accessibility in Bangladesh’s urban slums (Ahmed, 2014). According to the survey that I conducted where I asked people to rank the challenges that limit access to better healthcare services in urban slums, astonishingly, 78.6% confirmed that the reason why people cannot
access better healthcare services in urban slums is that they are poor as shown in Fig. 3.
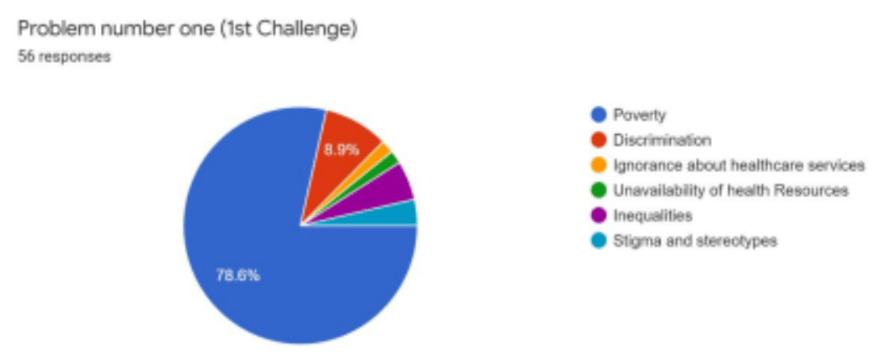
Fig. 3. Created by Author
Poverty has seeped into the centricity of urban slum dwellers as they struggle to access basic social services. According to the Daily Star, many of them are migrants to urban areas and their movement was spiked by the search for better employment opportunities, disaster relief, and changing climatic conditions. Due to the limited opportunities and infrastructures in urban areas, many of them are left without any opportunity to hold onto, and thus, become squatters along river banks giving rise to slums. Despite the fact that the resources and infrastructure in urban settings are limited and overlay constrained, it makes it hard for such groups to access a bare minimum of better healthcare services while in urban slums. Additionally, since the components of adequate healthcare take into account access to food, clothing, and shelter and ensure a stable mental state; transient living, environmental hazards, social fragmentation, exposure to crimes, violence, and accidents are key deprivations to better healthcare in the urban slums (Daily Star, 2015). Studies show that many households of the urban poor are food insecure (Environmental Health Project, 2004) besides which the living conditions are also evident as illustrated by the small cluttered houses, fires, flooding, and waterlogging which do not add up to better healthcare services. To sum up, Ahmed (2014) recommends Urban Partnerships for Poverty Reduction (UPPR) programs since they have recorded notable success in improving the lives of more than three million urban poor populations to overcome the poverty scourge.
The second notable challenge is ignorance about better healthcare services. Many people are off the radar to access better healthcare facilities because they lack knowledge about the existing facilities. The survey indicated that 32.1% of the poor urban slum population lacked knowledge about the various better healthcare incentive programs which are passed through the Community Health Workers and Organizational projects as illustrated in Fig. 4
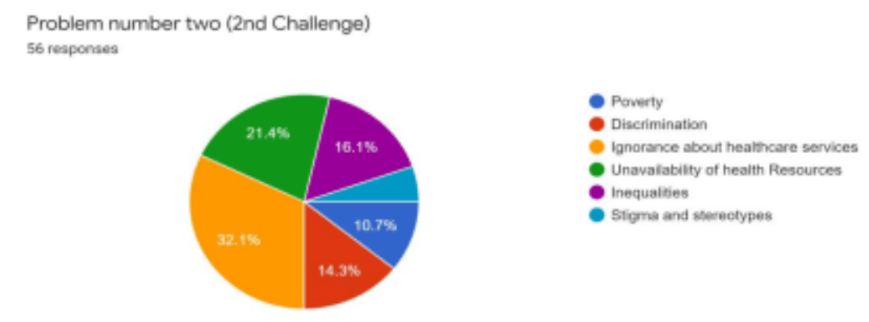
Fig. 4. Created by Author
The majority of the urban slum dwellers do not have basic or elementary education, which makes it difficult for them to be sensitized about good health practices such as joining Health clubs, and Urban Partnership for Poverty Reduction programs. As a result, they are fearful of the terms and conditions since they cannot easily interpret the essence of some opportunities and how they make their lives better. Studies also show that lack of access to education by the young adults limits their accessibility to quality decent work which in turn makes them unable to access better healthcare services. (Daily Star, 2014). According to a review by the Bangladesh Demographic and Health Survey, women with no education at all were unable to access better healthcare services compared to women with basic education (Hindawi, 2019). This, therefore, meant that there are lagging loops in the sensitization of people to the common language they understand. This can be illustrated in a case story of a slum habitat that was to be evicted from their settlement since the authorities had promised to send Land surveyors to landmark the area. However, humanitarian activists wanted to help and intervene in the situation by carrying out a community survey. Since the first impressions and communications were linked to making a survey, the Localities chased them away claiming that they were the promised people to demarcate them. The point is that language may not be convincing enough to kill ignorance in the people, hence, building on to nothing.
Last but not least, the unavailability of health resources is also a major challenge. 30.4%.
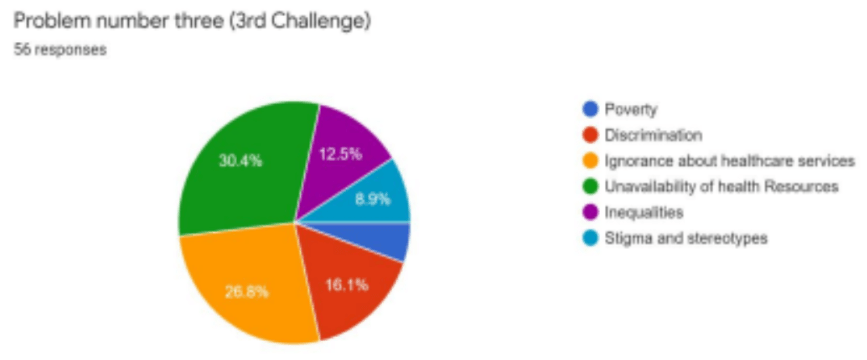
Fig. 5. Created by Author
A study on the global health workforce showed that Bangladesh suffers from both a shortage of skilled workforce and geographical maldistribution of Human Resources for Health, HRH (WHO, 2021). The study adds that there are an estimated 3.05 physicians for every 10,000 people and 1.07 nurses for every 10,000 people (MoHFW HRD, 2011). This implies that despite the population’s willingness to utilize better healthcare services, there is an acute crisis of healthcare providers making many fear utilizing the services. A crisis in Healthcare Providers (HCPs) implies the development of monopoly powers in the healthcare sector leading to high costs of attaining healthcare services. This is why many people still rely on unregulated drug clinics (The Lancet, 2013) since they offer relatively low-priced healthcare services regardless of their poor quality. Therefore, this means more workforce is needed as well as developing facilities to meet the needs of the poor populations that make up the slum majority. Factors like discrimination based on social class, inequalities, stigma, and stereotypes also contribute to limited accessibility of better healthcare services available to those living in urban slums.
Conclusion
The challenges that limit access to better healthcare access in urban slums are attributed to the government ministries, the urban slum population, the health workforce, and the non-government organizations. The variance is in the degree and extent to which these amounts to. Some of the policy recommendations state that the government should set a minimum and maximum cost for healthcare services especially in private settings, increase and expand the numbers of community health workers, enhance public and private partnerships, sensitize people about better healthcare practices, and equip community health workers with emergency toolkits to improve healthcare delivery.
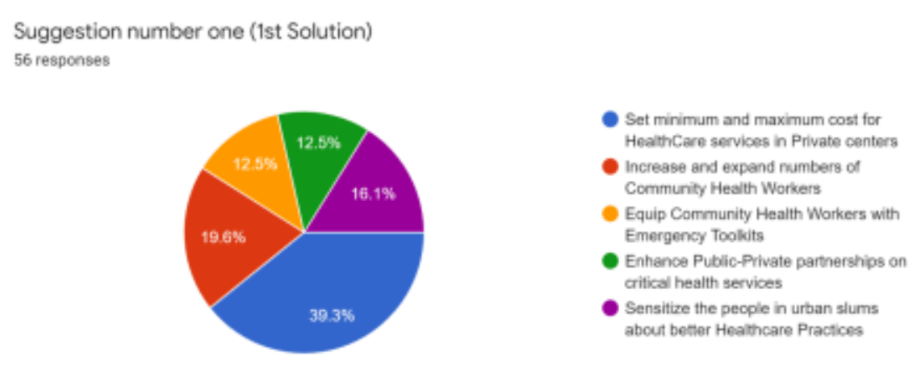
Fig. 6. Created by Author
References
Abed, F.H. (2013, November). Healthcare for poor people in urban slums of Bangladesh. The Lancet.
Afsana, K., & Wahid, S. S. (2013, December). Healthcare for poor people in the urban slums of Bangladesh. The Lancet.
https://doi.org/10.1016/S0140-6736(13)62295-3
Ahmed, I. (2014, September). Factors in building resilience in urban slums of Dhaka, Bangladesh. Procedia Economics and Finance.
Ahmed, M.S., Hossain, M.A. … & Bhiuya, A.U. (2011, January). The health Workforce crisis in Bangladesh: shortage, inappropriate skill-mix and inequitable distribution. Human Resource for health.
https://human-resources-health.biomedcentral.com/articles/10.1186/1478-4491- 9-3
Ahmed, N.U., Alam, M.M.… & Powers, M.B. (2006, December). Reaching the unreachable: barriers of the poorest to accessing NGO healthcare services in Bangladesh. National Library of Medicine.
Banik, K.B., & Sumon, M.S.R. (2018, August). Barriers to access maternal health service among urban poor women in Bangladesh: A Case of Rajshahi City. South East Asia Journal of Public Health.
Banks, N., Roy, M., & Hulme, D. (2011, October). Neglecting the Urban poor in Bangladesh: research, policy and action in the context of climate change. SAGE Journals. Environmental Health Project. (2004, August). Improving the Health of the urban poor: Learning from USAID Experience.
http://www.ehproject.org/PDF/Strategic_papers/SR12-
UH%20ImproveHealth.pdf
Islam, A., & Biswas, T. (2014, November). Health System in Bangladesh: Challenges and Opportunities. American Journal of Health Research.
Joarder, T., Chaudury, T.Z., & Mannan, I. (2019, March). Universal Health Coverage in Bangladesh: Activities, Challenges and Suggestions. Hindawi.
Khan, A.A.M. (1982, October). Rural-Urban Migration and Urbanization in Bangladesh. The Geographical Review.
Kin, O.M. (2020, September). The Health Challenges for the urban poor. The Daily Star.
Mannan, M.A. (2013, December). Access to Public Health facilities in Bangladesh. A study on Facility Utilization and Burden Treatment. Bangladesh Development Studies. Shahen, M.A., Islam, M.R & Ahmed, R.(2020, January). Challenges for Health care Services in Bangladesh: An Overview. IOSR Journal of Nursing and Health Science. The World Bank. (2018, March). Health and Nutrition in Urban Bangladesh. https://www.worldbank.org/en/country/bangladesh/publication/health
nutrition-urban-bangladesh
UN-Habitat. (2008). Case Study: Dhaka’s Extreme Vulnerability to Climate Change, United Nations Human Settlements program, Nairobi.
World Health Organization. (2021). Global Health Workforce Alliance: Bangladesh.